Medicare Final Rule Changes That Home Health Providers Need To Know
The Medicare home health final payment rule for calendar year 2026 has been most discussed for its methodology and its 1.3% aggregate rate cut, but other aspects of the final rule require home health providers to carefully strategize for the upcoming year.
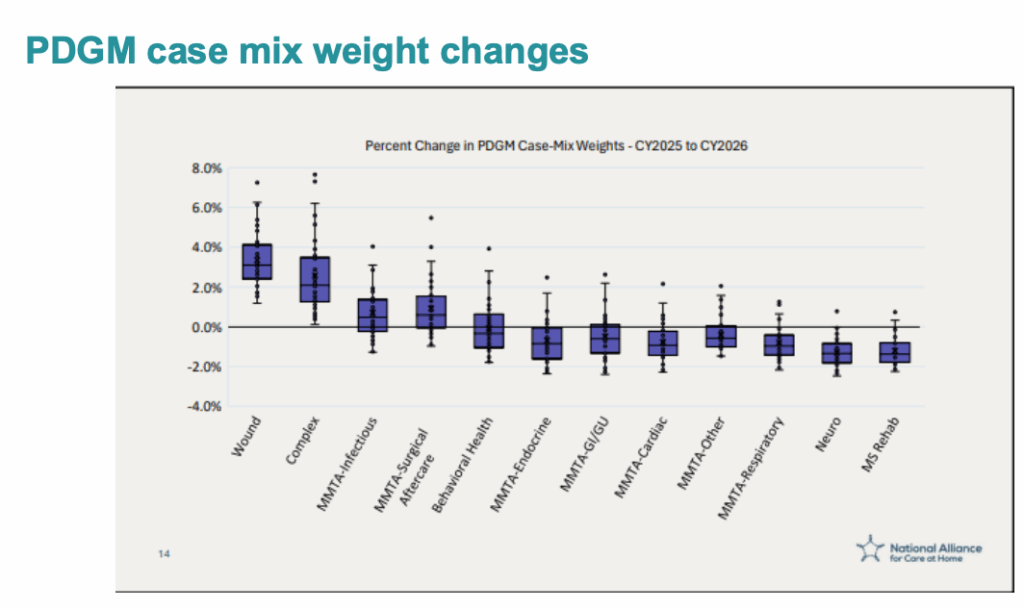
In the final rule, the Centers for Medicare and Medicaid Services (CMS) recalibrated all 432 PDGM case-mix weights and associated low utilization payment adjustment (LUPA) thresholds using utilization data from calendar year 2024. This recalibration shifts payments away from certain PDGM groups and toward others, and ultimately rewards coding accuracy of higher-acuity patients, according to a webinar hosted by WellSky.
Overland Park, Kansas-based WellSky is a health care technology company serving over 20,000 client locations, including hospital systems, home health and hospice operations and other post-acute providers.
In 2026, it will be key for providers to determine their case-mix weights and how to work with different PDGM groups, according to Cindy Campbell, senior director of advisory services at WellSky.
Some case mix weights rose and some decreased. A high-acuity 30-day period classified as early, community, high functional, crossover comorbidity may see its case-mix weight increase, and therefore increase payment.
A low-acuity, 30-day period classified as late, institutional, low functional, no comorbidity, meanwhile, may see its case-mix weight decrease, lowering payment.
Among the rule changes is a shift in LUPA thresholds. The change is relatively small, only one visit, but it requires providers’ attention, Campbell said. The shift means that providers must be especially careful to perform comprehensive assessments every 60 days.
“If you have specific groups of patients, for example, if we had cardiopulmonary or orthopedic groups, in ‘25 those LUPA thresholds may have been four visits,” Campbell said. “Those groups may have been bumped up to five. Other groups … may have been decreased by one visit down to one.”
For other patients, such as long-term once-a-month Foley catheter patients, it can be tempting to think that nothing needs to change and providers can therefore skip the 60-day assessment. But reassessing and reiterating the care plan ensures that workers are aware of changes in the patient’s body over time, which can impact the need for further intervention.
In the future, as new technology becomes available, tools like generative AI and ambient listening can ensure comprehensive assessments, not patient history, guide future low utilization payment adjustments, Campbell said.
The final rule also changed the face-to-face encounter, finalizing a change that allows physicians other than the certifying practitioner or the physician who cares for the patient in the location from which the patient was directly admitted to home health. The intent of the change is to ensure that the physician or allowed practitioner conducting the face-to-face encounter is the most knowledgeable with firsthand information about the patient’s current clinical condition, according to the webinar.
The rule also revised the Consumer Assessment of Healthcare Providers and Systems Home Health Care Survey (HHCAHPS), to begin with the April 2026 sample collection.
CMS added three new questions that include asking whether the care provided helped the patient take care of their health, whether the patient’s family or friends were given sufficient information and instructions and whether the patient felt the staff cared about them “as a person.”
The number of medication questions was decreased to two and questions that were not used in public reporting composites were removed. Two composite measures remained but were altered, and three new standalone measures took the place of the special care composite measure.
Additionally, CMS removed the COVID-19 vaccination assessment, though providers must complete the OASIS item until April 1, and removed four social determinants of health assessment items.
Still, some of these changes to HHCAHPS may not last forever.
“As CMS works to align different data elements and staff them, they know that they’re very important to the relative outcomes and spending of the program; however, they also know that right now, we are gathering too much, so they will need to align it,” Campbell said. “We would not be surprised to see them integrated in future years, coming back.”
The post Medicare Final Rule Changes That Home Health Providers Need To Know appeared first on Home Health Care News.
Popular Products
-
 Lightweight Auto Cane Grab Handle
Lightweight Auto Cane Grab Handle$38.99$26.78 -
 Plug-in Carbon Monoxide Detector
Plug-in Carbon Monoxide Detector$57.99$39.78 -
 Universal Baby Safety Stove Knob Covers
Universal Baby Safety Stove Knob Covers$30.99$20.78 -
 King Size Bed Wedge Pillow
King Size Bed Wedge Pillow$157.99$109.78 -
 Detachable Hydraulic Patient Lift Chair
Detachable Hydraulic Patient Lift Chair$801.99$479.78